Select Important Safety Information
Who should not take Hemady®?
Do not take Hemady® if you:
- Are allergic to Hemady® or any of the ingredients in Hemady®.
- Have an infection inside your body. Hemady® may make it worse.
How should I take Hemady®?
Your doctor will tell you how to take Hemady® based on the treatment regimen in the other anti-myeloma product prescribed for you.
What are possible side effects with Hemady®?
Hemady® can cause serious side effects including:
Alterations in endocrine function (hormones). This is especially important in patients with diabetes as Hemady® can cause blood glucose levels to rise. Your healthcare provider may monitor glucose levels more frequently. If you have diabetes, talk to your healthcare provider as adjustments in your diabetes medications may be needed.
An increased risk of infection. Hemady® can suppress your immune system. Tell your healthcare provider if you have had any recent or ongoing infections and if you develop any sign of infection while taking Hemady®. Avoid live or live attenuated vaccines.
An increase in blood pressure, salt and water retention, and potassium and calcium excretion. Speak to your healthcare provider to discuss monitoring blood pressure and identifying signs of fluid retention and loss of potassium, especially if you have congestive heart failure, a recent heart attack, or hypertension.
Blood clots in your arteries, veins, and lungs, heart attack, and stroke can happen if you take Hemady® and the risk may be greater when taking Hemady® with other anti-myeloma drugs. Your doctor may prescribe a blood thinner medicine to help prevent clots.
Hemady® may cause cataracts or glaucoma. Your healthcare provider may monitor you for these effects.
Increase the risk of developing gastrointestinal perforation. Promptly seek medical attention if you develop unusually severe, persistent or worsening abdominal pain.
Prolonged use of Hemady® can cause osteoporosis, which can lead to bone fractures.
Unexplained muscle pain, tenderness, or weakness. If you experience these effects, contact your healthcare provider, it may be a condition known as myopathy.
Irritability, mood swings, personality changes, and severe depression. Hemady® can also cause insomnia. Inform your healthcare provider if you notice behavioral and mood changes or have experienced difficulty sleeping.
Risk of Kaposi’s sarcoma. Corticosteroids can cause Kaposi’s sarcoma. Stop taking Hemady® if Kaposi’s sarcoma is diagnosed.
Adverse reactions can occur when Hemady® is taken in combination with anti-myeloma products.
Certain medications can cause an interaction with Hemady®. Tell your doctor about all the medicines you are taking, including over-the-counter medicines, dietary supplements, and herbal products.
Corticosteroids, including Hemady®, can cause fetal harm. Women should not become pregnant while taking Hemady® and for one month after stopping Hemady®. Talk to your healthcare provider if you are pregnant or are planning to become pregnant. Women should not breastfeed while taking Hemady® and for two weeks after the last dose.
These are not all the possible side effects of Hemady®. Call your Healthcare Provider for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088 (1-800-332-1088). You also may contact Edenbridge Pharmaceuticals, LLC at 877-381-3336.
Please see Full Prescribing Information for Hemady®.
Hemady® [Prescribing Information]. Edenbridge Pharmaceuticals, LLC. June 2024.
References
- Hemady® [Prescribing Information]. Edenbridge Pharmaceuticals, LLC. June 2024.
- FDA. Center for Drug Evaluation and Research. Hemady New Drug Application. 2019.
- Rosenberg AS. Leuk Lymphoma. 2023;64(2):283-291. doi:10.1080/10428194.2022.2136950.
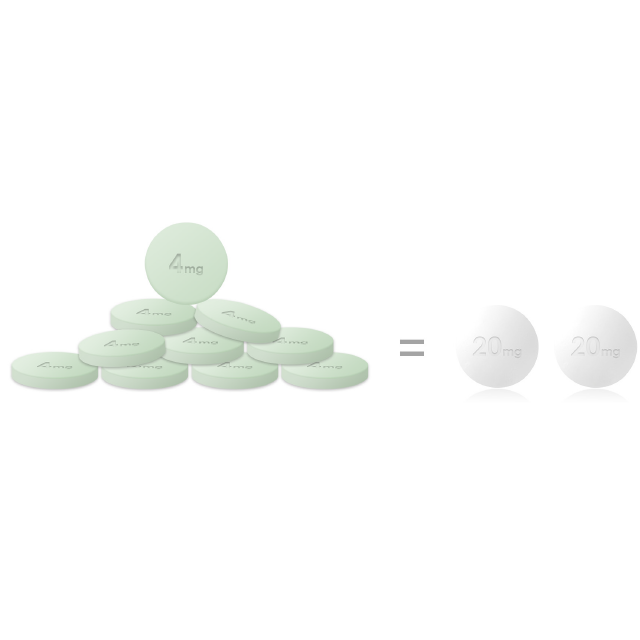
- Data on file (Pill size correspondence). Edenbridge Pharmaceuticals, LLC. 2020.
- Bashir Q, et al. Clin Lymphoma Myeloma Leuk. 2020;20:768-7735.
- Harrison SJ, et al. Am J Hematol. 2015;90:E86-E91. Epub February 27, 2015. doi:10.1002/ajh.23967.
- Sinha S, et al. Br J Haematol. 2010;148(6):853-858. doi:10.1111/j.1365-2141.2009.08023.
Information provided on this website is not a substitute for talking with your doctor.
Your doctor is the best source of information about your disease.
All individuals depicted are models used for illustrative purposes only.